Coronary angioplasty is an intervention that enables repair of a narrowing (i.e. stenosis) or occlusion of a coronary artery linked to cholesterol / fat deposition (atheroma) in the arterial wall. It restores normal blood flow through the arteries of the heart and thus has become an alternative to open heart surgery. It is often performed just after the coronary angiogram during the same setting or can be postponed. In certain cases, it is performed in an emergency setting, notably in the event of a heart attack.
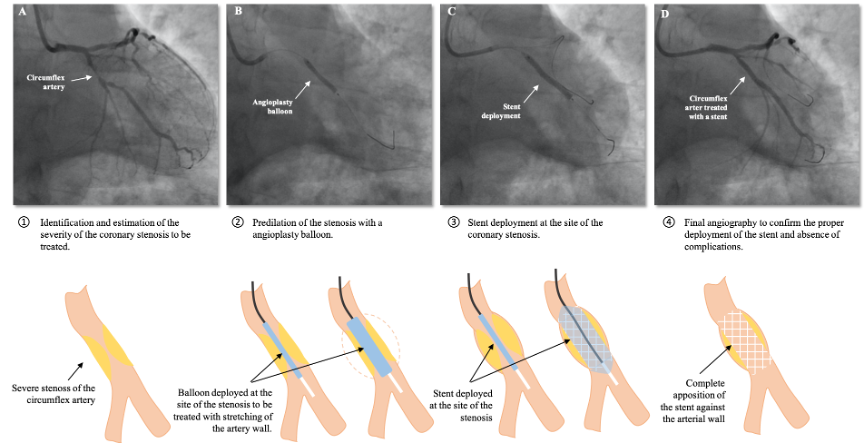
The intervention consists in crossing a coronary artery narrowing with a very thin metal guidewire and then bringing a balloon which will be locally inflated to spread the wall of the diseased artery and cause the narrowing to yield. After removing the balloon, the interventional cardiologist puts in place a small metal prosthesis (stent) which will stabilize the dilated artery and improve long-term results.
How does a coronary angioplasty take place?
A 24 to 48 hours hospitalization is required.
It is often performed just after the coronary angiogram. If deferred, its course will be identical to the coronary angiogram that you will have had a few days before.
The day before the procedure, you will be given blood thinners (antiplatelet agents) to prevent clot formation in your stent(s).
After the anesthesiologist has injected medication to relax you, the procedure is performed under local anesthesia.
A catheter, most commonly inserted from the wrist (radial artery), is brought to your coronary artery and a metal guidewire is then inserted into your diseased artery, guided by X-ray and iodinated contrast agent.
A balloon is inflated to remove the obstruction created by the atherosclerotic plaque. Inflation of the balloon can sometimes be accompanied by brief chest pain identical to that experienced during exertional angina.
After ensuring the disappearance of the narrowing, the doctor then introduces a stent, appropriately sized for length and diameter according to the length of the stenosis to be treated as well as the diameter of your coronary artery.
At the end of the procedure, the guidewire and catheter are removed, and the puncture site is compressed with a pressurized bracelet. The bracelet is gradually deflated over the following hours.
You will be authorized to leave the clinic the next morning, following the interventional cardiologist’s visit. The doctor will indicate the ideal timing to go back to work and to resume physical activities/sports and/or prescribe a medical leave, if indicated.
You will be given a prescription prior to your discharge from the clinic, which will include a combination of antiplatelet agents (“blood thinners”) prescribed for several months which should never be interrupted without the advice of your treating cardiologist or a doctor from CCI Belledonne.
Certain complementary techniques can be used during the procedures, depending on the complexity of the lesions to be treated:
- Rotational atherectomy: device that allows sanding of the atheroma plaque in the presence of resistant calcifications.
- Cutting balloon: balloon fitted with specific metal blades that shears atheroma plaques.
- Drug-eluting balloon: balloon coated with a specific drug preventing cell proliferation and reducing the risk of restenosis – used for in-stent restenosis and in arteries of small caliber.
- Intracoronary imaging: imaging probe that enable visualization of the arterial wall in order to measure its diameter and to understand the underlying mechanism involved in myocardial infarction.
- Intracoronary physiology – FFR (fractional flow reserve): guidewire with a pressure sensor to objectively evaluate the hemodynamic impact / severity of a coronary stenosis, especially in cases of intermediate narrowings.
What’s a coronary stent and how does it work?
A stent is a prosthesis composed of a metal platform coated with a specific drug. Coronary stents are used to allow proper healing of an artery and to avoid the rapid appearance of a new stenosis. We currently use the latest generation of drug-eluting / active stents, which have the property of delivering a specific antiproliferative drug to the arterial wall to be treated. Thus, the risk of restenosis or development of a new narrowing is less than 8%.
Since it is a metallic platform, there is a risk of clot formation inside the stent until the healing process is complete. A treatment composed of 2 different antiplatelet agents (“blood thinners”) will be prescribed for several months upon discharge from the clinic. This treatment will be reduced in time by your treating cardiologist during follow-up.
Is it dangerous?
Complications related to a coronary angioplasty are the same as that of the diagnostic coronarography. Our interventional cardiology team and anesthesiologists put everything in place to minimize and avoid the risks of complications. They have at their disposal all the tools needed to repair the arteries that could be damaged during the intervention. Exceptionally (1 case in 1000), a complication can lead to another angioplasty, emergency cardiac surgery, a myocardial infarction or death. Fortunately, these complications are extremely rare.
All the potential complications are fully detailed in the informed consent form for the exam given upon entry and to be signed before the procedure.
In summary
- Hospitalization for 12 to 24 hours
- The mean duration of the procedure: 20-45 minutes
- The intervention is painless for the majority of patients.
- A 24-hour surveillance on monitors is required. In absence of symptoms and/or bleeding at the puncture site, the patient can leave the clinic the next morning, following the interventional cardiologist’s visit.
- Rigorous compliance to the medical treatment is essential.
- Follow the recommendations given on discharge from the clinic.