What is a TAVI procedure?
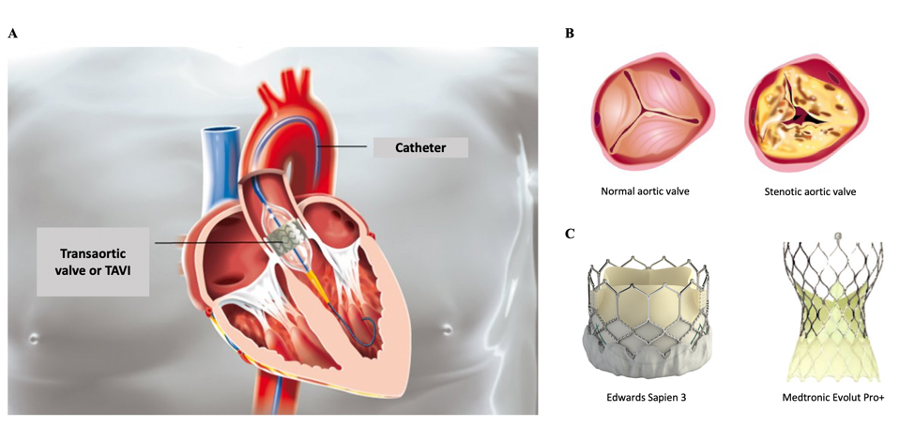
It is a percutaneous endovascular technique of aortic valve replacement that has proven to be an effective alternative treatment to aortic valve replacement by conventional open-heart surgery for many patients, particularly the elderly, frail and those suffering from multiple other medical conditions.
The concept is simple and revolutionary: it consists in introducing a prosthesis through a diseased aortic valve using a catheterization system that avoids surgical cut-down, extracorporeal circulation or stopping the beating heart.
Which patients are offered this intervention?
TAVI is intended for patients with a tight narrowing of the aortic valve (i.e. aortic stenosis (AS)). The aortic valve ensures forward blood flow from the left ventricle (cardiac pump) through the aorta and general circulation. As we get older, the valve thickens and calcifies, which can gradually cause an obstacle to blood flow (narrowing); the valve can no longer open normally with each heartbeat. This chronic disease is well tolerated for years until the warning signs appear (shortness of breath, chest pain, lightheadedness or loss of consciousness), with a high-risk of mortality from sudden cardiac death or heart failure at 2 to 3 years without specific treatment.
AS is a common disease that increases in prevalence with age, affecting 10% of those over 70 years-old and 15% of those over 80 years old. Currently, patients that are eligible for a TAVI procedure are those with symptoms and who are either surgically inoperable or are deemed to be at high-risk for surgery. They are selected by the attending cardiologist that will confirm the degree of severity of AS by echocardiography. Clinical indication for TAVI procedure will be confirmed following a 48-hour complete workup at the Clinique Belledonne, including a diagnostic coronary angiogram and cardiac catheterization, CT scan of the aorta and femoral arteries and a geriatric consultation.
Which prosthetic valves do we implant?
With TAVI, an artificial tissue valve (bioprosthesis) is implanted. It is made of animal (bovine, porcine) pericardium (thin membrane surrounding the heart), reproducing the shape of a normal human aortic valve, and fixed to a tubular and a balloon-expendable metallic mount. These prosthetic valves are comparable to those implanted surgically that are known to have excellent long-term reliability.
Where and how does a TAVI take place?
Interventional cardiologists of the Clinique Belledonne perform their TAVI procedures at the Centre Hospitalier Universitaire (CHU) de Grenoble. The procedure is performed in an aseptic catheterization laboratory under local anesthesia and sedation or mild general anesthesia. Through a small cutaneous opening at the groin, a catheter containing the prosthesis in a compressed form is introduced into the femoral artery. The catheter is brought retrogradely into the aorta to the middle portion of diseased aortic valve before the prosthesis is deployed under X-ray guidance. When deployed, the prosthetic valve anchors to the calcified edges of the native diseased valve. In cases where the caliber of the femoral artery is too small, an alternative surgical approach is selected for the procedure.
In summary
- Hospitalization for 24-48 hours.
- Mean duration of the intervention: 30-45 minutes
- The intervention is painless for most patients.
- After 2 to 3 days under close surveillance/monitoring, including an overnight stay at the intensive care unit, the patient is discharged home.
- Regular follow-up with your treating cardiologist is necessary and an antiplatelet agent will be prescribed for several months.
- Rigorous compliance to the medical treatment is essential.
- Moderated physical activities can be resumed quickly.
What are the expected results and benefits of a TAVI procedure?
Immediate success rate of TAVI bioprosthesis currently exceeds 90% with a rapid improvement of symptoms (shortness of breath, fatigue and lightheadedness) and in quality of life. This intervention also significantly improves heart function and markedly increases life expectancy. Studies have shown that TAVI decreases the mortality rate by 50% in comparison to optimal medical therapy alone and that it rivals open-heart surgery interventions in patients with intermediate, high or prohibitive surgical risk.
What are the immediate procedural risks?
The mortality rate related to this procedure is constantly declining due to increasing experience of medical teams and operators, as well as improvement of the equipment. It is currently low (1 to 3% at 30 days) if patients have good baseline health status without other severe diseases. In addition to the complications linked to the catheterization procedure itself, there are specific procedural complications, including prosthesis malapposition with residual leakage, cardiac conduction disorders requiring pacemaker implantation (10-15% of cases) and laceration / trauma of the femoral artery requiring immediate surgical repair. The occurrence of a stroke, in most cases of minor severity, is observed in 3% of cases.
TAVI in the future ?
New prostheses are developed from synthetic or biologic materials that form an airtight mold limiting the risk of blood leakage around the valve after implantation. They are more easily compressed in the catheter, which facilitates their introduction in the femoral artery even of small caliber. In view of excellent mid-term results at follow-up, the indications for TAVI are gradually extending today to younger patients and those at lower surgical risk. Thus, it is not unrealistic to envision that this technique could become the reference procedure for the treatment of all severe aortic stenoses in the near futur, surpassing surgery.