Cardiac catheterization is performed at the same time as the coronary angiogram. It is a method of invasive hemodynamic exploration consisting in measuring pressures and oxygen saturation levels of the blood in various cavities of the heart and vessels under X-ray guidance. The indications to perform a cardiac catheterization are to evaluate the presence and importance of specific cardiac pathologies such as:
- Narrowing or leaking of a heart valve
- An anomaly of the blood trajectory in the heart, called intracardiac shunt
- Pulmonary arterial hypertension (PAH)
- Heart failure
- Detailed assessment of your condition prior to heart surgery
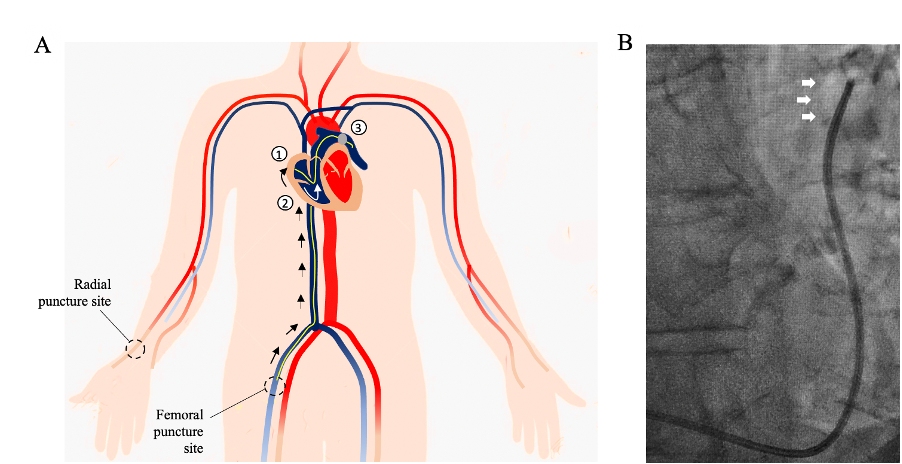
The exam consists in introducing catheters into heart chambers under local anesthesia. Two punctures are most often performed: by the femoral vein (groin) for the catheterization of the right cavities and by the radial artery (wrist) for the catheterization of the left cavities. The interventional cardiologist measures the pressures in all the cardiac chambers.
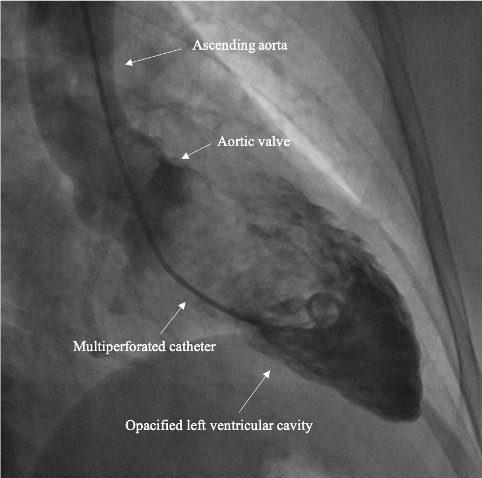
He then completes the exam with a left ventriculography, which assesses the ability of the heart muscle to contract. To do this, the interventional cardiologist injects an iodinated contrast media using a multiperforated catheter positioned in the cavity to be studied. The injection of the contrast agent can produce a brief and migratory sensation of heat. This part of the exam also assesses the presence of aortic or mitral valve anomalies.
In summary
- Hospitalization for 12 to 24 hours.
- Puncture at the wrist and groin.
- The mean duration of the exam: 30-40 minutes.
- The exam is painless for the majority of patients.
- A 6-hours immobilization period following the cardiac catheterization is required in order to avoid bleeding at the puncture sites.
- Strenuous physical effort is discouraged for 72 hours following the procedure to avoid bleeding at the radial and/or femoral puncture site.