Angioplasty of the left main coronary artery
Severe stenosis of the left main coronary artery is defined by a narrowing of at least 50% of the internal diameter of the artery. It is found in 4-6% of patients undergoing diagnostic coronary angiogram and is frequently associated with disease in other coronary arteries. This is the most severe disease of the coronary artery tree given the risk of sudden cardiac death. Stenosis of the left main can occur at its origin (ostium), its mid-portion or its distal end. Clinical symptoms associated to a left main stenosis are shortness of breath, chest pain and dizziness related to a drop of blood pressure. The diagnosis is quickly made during the coronary angiography.
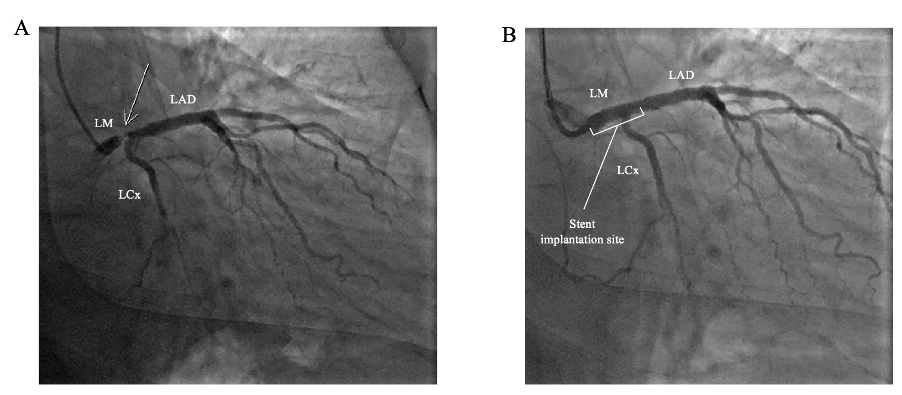
The sole treatment for left main coronary artery stenosis has long been cardiac coronary bypass surgery. Nowadays, coronary angioplasty has become an alternative of choice for the treatment of left main stenosis in selected patients.
The decision to proceed with revascularization of the left main coronary artery by angioplasty rather than by coronary bypass surgery is always made, in a non-urgent setting, after consultation with your cardiologist, the interventional cardiology team and other doctors. The decision will be based on the anatomy of the left main, the extent of the coronary artery disease, the presence of diabetes, the ability of your heart to contract and your surgical risks.
Thus, angioplasty of the left main is always performed (in a non-urgent setting) a few days following the diagnostic coronary angiography in order for the team to discuss your case and to explain the benefits and risks of the revascularization strategy. Several techniques exist to repair the left main coronary artery, but most often the interventional cardiologist will only need to implant 1 drug-eluting stent.
It is dangerous?
Complications related to a coronary angioplasty of the left main are the same as that of the coronary angiography.
In summary
- Intervention that is performed in selected patients.
- Hospitalization for 24 to 48 hours.
- Mean duration of the exam: 30-45 minutes
- The exam is painless for the majority of patients.
- A 24-hour surveillance on monitors is required. In absence of symptoms and/or bleeding at the puncture site, the patient can leave the clinic the next morning, following the interventional cardiologist’s visit.
- Rigorous compliance to the medical treatment is essential.
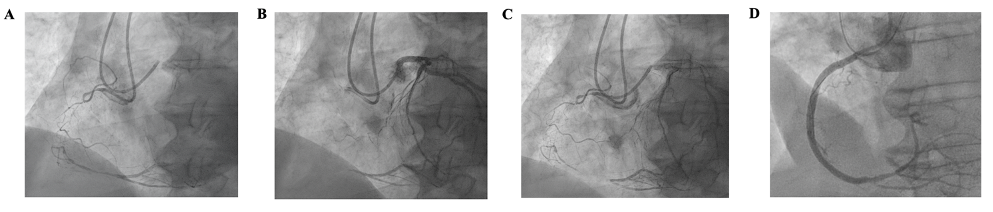
Recanalisation of a chronic total occlusion (CTO)
Chronic total occlusions (CTOs) are coronary lesions that have become completely blocked for at least 3 months. The CTOs are identified in approximately 20% of patients undergoing a diagnostic coronary angiogram. Although a natural bypass system called collateral circulation develop to provide adequate blood flow to the heart muscle supplied by the CTO, there are cases whereby the collateral arteries are insufficient to supply the heart muscle adequately. It is the case of patients experiencing chest pain or shortness of breath despite optimal medical therapy or in those with a significant lack of oxygenation to the heart visualized during a stress tests (cardiac perfusion scan, stress echocardiography, cardiac MRI).
Recanalization of a CTO can be technically challenging due to the length of the occlusion as well as the fibro-calcified nature of the lesion. It requires the use of dedicated material and specific techniques. In order to visualize the distal part of the blocked coronary artery, the procedure requires to go through both wrists or by the wrist and groin simultaneously. The intervention success rate is slightly lower than for standard coronary angioplasty.
It is dangerous?
Complication rates remains low when procedures are performed by experienced operators such as the interventional cardiologists of the CCI Belledonne. The risk of death is estimated at 0.2%, emergency coronary bypass surgery at 0.2%, stroke at 0.01% and myocardial infarction at 2.5%.
In summary
- Intervention is performed in selected patients when clinically indicated.
- Requires going through both wrists or wrist/groin (2 puncture site).
- Hospitalization for 24 to 48 hours.
- Mean duration of the intervention: 45-80 minutes
- The exam is painless for the majority of patients.
- A 24-hour surveillance on monitors is required. In absence of symptoms and/or bleeding at the puncture site, the patient can leave the clinic the next morning, following the interventional cardiologist’s visit.
- Rigorous compliance to the medical treatment is essential.